Prolapsed Haemorrhoids
▶What are the signs and symptoms of prolapsed haemorrhoids?
▶How are prolapsed haemorrhoids treated?
When haemorrhoids get larger and protrude outside of the bottom they can become very sensitive and painful. Find out what causes them, how you can recognise them, and what treatment options there are.
What are the signs and symptoms of prolapsed haemorrhoids?
Haemorrhoids are veins inside and around your bottom that have become enlarged and swollen. They are also sometimes called ‘piles’ and are more common than you might think, affecting 3 out of 4 adults.
Prolapsed haemorrhoids are those that are no longer contained within the bottom but push outwards and become exposed. They can be very sensitive and painful particularly when sitting down or during a bowel movement and can happen to internal haemorrhoids that originate inside the passage as well as external haemorrhoids (those nearer to the anus).
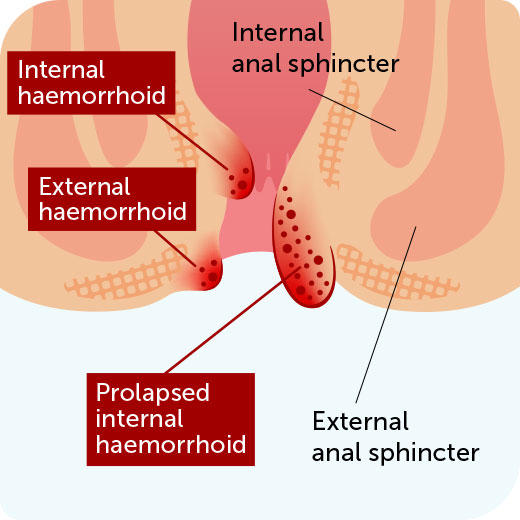
Internal haemorrhoids are classified according to whether they come out of the bottom and how far they protrude:
▶First degree piles may bleed but don’t come out
▶Second degree piles come out after a bowel movement but go back inside on their own
▶Third degree piles come out and don’t go back inside unless you push them in
▶Fourth degree piles always come out, are very painful and can’t be pushed back in.
In addition, you may notice some of the other symptoms associated with haemorrhoids:
▶Small lumps bulging out from the anus (there can be one or more of these)
▶Pain during bowel movements
▶Mucus in the stool
▶Bright red blood after a bowel movement
▶An itchy bottom (anus)
▶The feeling of still needing to go to the toilet.
Prolapsed Haemorrhoids
A haemorrhoid typically becomes prolapsed when the connective tissue holding it in place is weakened. This can happen for a number of reasons common to other types of haemorrhoids too, for example:
▶Too much straining when going to the toilet
▶Constipation - difficulty with bowel movements can result in over-straining
▶Diarrhoea – frequently needing to go to the toilet can put pressure on blood vessels
▶Spending a long time on the toilet (e.g. due to constipation or diarrhoea)
▶A low fibre diet – insufficient fibre in your diet can make stools harder and more difficult to pass
▶Over-exertion – lifting heavy weights or over-exercising can also put strain on the blood vessels around the bottom
▶Obesity – carrying extra body weight can put a strain on your body
▶Pregnancy – the pressure of an enlarged uterus and hormonal changes can relax the blood vessels
▶Older age – as we get older the tissues holding haemorrhoids in place become weaker.
The good thing is that many of these causes can be managed to help you avoid developing piles again in the future. There are also a number of treatment options that can provide welcome relief from the unpleasant symptoms.
How are prolapsed haemorrhoids treated?
Even though prolapsed haemorrhoids come out of the bottom, you may be able to carefully push them back in yourself. They can also go back inside on their own but, if left untreated, they may develop into thrombosed haemorrhoids or become strangulated if the blood supply is cut off. Both of these scenarios can be very unpleasant and may require treatment from a doctor so it’s worth addressing them early on.
Generally speaking, the treatment options for prolapsed haemorrhoids are the same as those for other types and include:
▶Home remedies such as a warm bath or ice pack applied to the area
▶Over-the-counter creams, ointments, and suppositories such as Germoloids
▶Non-surgical procedures such as banding
▶Surgical methods of removal.
You can read more about these on the Treating Haemorrhoids page.