Treatment for Haemorrhoids (Piles)
Haemorrhoids (also known as piles) can be itchy, uncomfortable and even painful in some cases. Fortunately, however, there are several treatment options available to relieve your symptoms.
What are the treatment options for haemorrhoids (piles)?
If you’ve ever suffered from haemorrhoids, you will have likely experienced the common symptoms that come with the condition first-hand, including bright red blood after a bowel movement, itching, pain and general discomfort around the bottom.
In many cases, haemorrhoids will often get better on their own after a few days. But, for some people, the itchiness, pain and discomfort can be hard to deal with and may require additional treatment from a pharmacist or doctor.
The main treatment options for piles typically include:
▶Home remedies and lifestyle changes
The NHS recommends that you should see a doctor if you have symptoms that show no sign of improvement after seven days, you keep getting piles or you notice a change around your anus that isn’t normal for you. This is because you might need to have a different medicine or treatment prescribed for your symptoms and to check that another issue isn’t causing them to appear.
Aside from the physical discomfort, many people also feel uncomfortable or embarrassed when talking about piles. But it’s important to realise that you’re not alone, with the condition estimated to affect around 10% of adults globally.
Which haemorrhoids (piles) treatment is best for me?
Determining the right treatment option for you will depend on the size, severity and type of haemorrhoids you have – internal or external.
External haemorrhoids typically cause itching, pain and/or one or more hard, tender lumps to appear around or near your bottom (anus).
On the other hand, internal haemorrhoids develop in the upper two-thirds of the anal canal. They tend to be associated with symptoms like bleeding from the rectum and prolapsing (piles that fall through the anal opening), which can cause pain and discomfort.
Internal and external haemorrhoids can also become what’s known as a thrombosed haemorrhoid. While this is usually associated with external haemorrhoids, thrombosed haemorrhoids are a common complication of piles and can cause extreme pain.
If your haemorrhoids need further examination, your doctor will be able to determine their exact type and size through a digital rectal examination (DRE).
A DRE is an internal examination where your doctor will wear gloves and a lubricant to feel for any abnormalities in your bottom.
If required, they may also perform what’s known as a proctoscopy to confirm your diagnosis. This is another type of internal examination that involves using a proctoscope (a hollow tube with a light at the end of it) to examine your rectum and anus.
Using the results of one, or both, of these tests, your doctor will be able to advise you on their recommended course of treatment.
Some people with haemorrhoids are reluctant to see their doctor, but there’s no need to be
embarrassed – all GPs are used to diagnosing and treating piles.
Home remedies and lifestyle changes
Several home remedies can help ease some of the symptoms of haemorrhoids when they first appear. You can help relieve symptoms of piles by:
- Taking paracetamol
- Having a warm bath
- Wrapping an ice pack in a towel before applying it to the painful area
- Wiping your bottom softly with damp toilet paper
- Gently pushing the pile back inside
- Keeping your bottom clean and dry
However, since lifestyle habits like diet and weight are some of the key risk factors for haemorrhoids, there are several other things you can do to help prevent them from coming back.

Drink more water
Keeping hydrated helps to soften stools, making them easier to pass and reducing the overall strain put onto your rectum and anus. This can not only help prevent the future development of haemorrhoids but also help alleviate any discomfort you currently have, by allowing the fibre you eat in your diet to work more effectively.
Eat more fibre
Incorporating higher-fibre foods like fruits, vegetables, beans and grains into your diet may help keep your digestive system running smoothly.
Exercise regularly
Performing regular exercise promotes colon health and may prevent constipation. However, it’s important to choose the right exercise, as certain types may make the problem even worse.
Exercises like walking, swimming and yoga, for example, are all generally considered helpful and effective.
Reduce your caffeine intake
If constipation could be a contributor to your haemorrhoids, you should also avoid any drinks that contain caffeine (such as tea, coffee or cola) and keep yourself hydrated by drinking plenty of water instead.
Over-the-counter creams, ointments or suppositories
If you find that home remedies aren’t helping your symptoms, you should speak to your doctor for advice on any over-the-counter medications you could use.
These types of haemorrhoid treatment come in a variety of formats, including creams, ointments and suppositories (which are inserted into your bottom), and are available from pharmacies without needing a prescription.
Certain over-the-counter remedies also include an anaesthetic to help provide symptomatic relief of the pain, swelling, irritation and itching often associated with haemorrhoids.
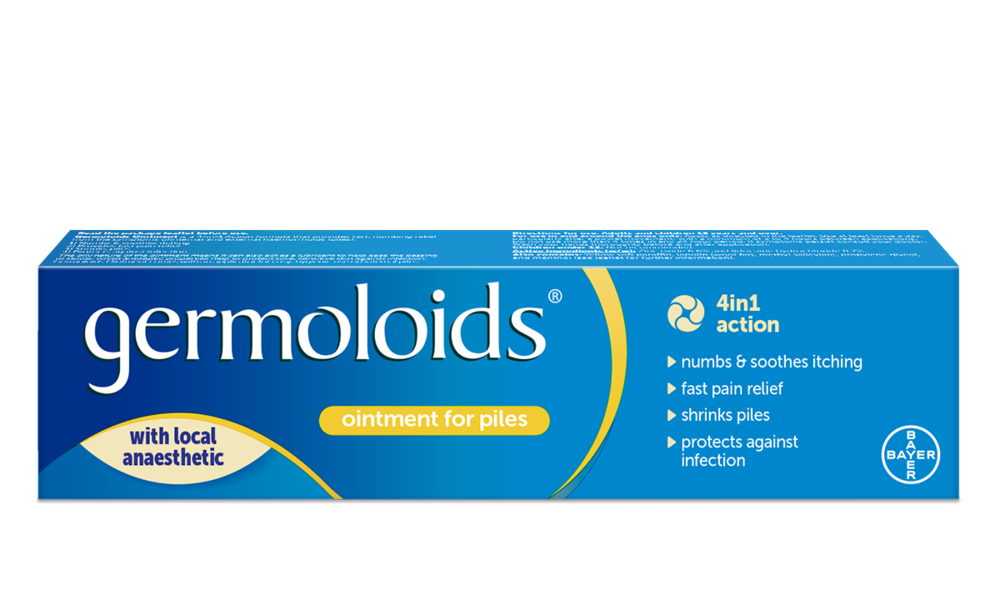
Take Germoloids®, for example. Unlike other types of over-the-counter remedies, all Germoloids® products are designed to contain a local anaesthetic, which can act quickly to provide fast, numbing relief from haemorrhoids.
Germoloids® is also available in different formats for use on internal or external piles. See below to discover the full range of products.
You can also use painkillers like paracetamol to help relieve the pain of living with haemorrhoids. But you should avoid using non-steroid anti-inflammatory drugs (such as ibuprofen) if your piles are bleeding, as they can make rectal bleeding worse. You should also avoid using codeine painkillers because they can cause constipation.
If you find that your symptoms persist or worsen after taking any of these over-the-counter medications, it’s always best to speak to your doctor for their advice.
Non-surgical procedures
If dietary changes and medication don’t improve your symptoms, your doctor may decide to refer you to a specialist for further diagnosis and, if necessary, possible non-surgical treatments. This could involve:
Injections or ‘sclerotherapy’
Treating haemorrhoids through a series of injections is known as sclerotherapy.
During this procedure, liquid containing medication designed to shrink the swollen blood vessels is injected into the haemorrhoid.11,14 This helps to reduce blood flow to the affected area(s), relieve pain, numb the injection site and, ultimately, cause the haemorrhoid to reduce in size and shrivel up.
Using this technique will also usually take between four and six weeks for the results to be seen.
Rubber band ligation
Rubber band ligation is another non-surgical solution used to remove haemorrhoids.
During the procedure, the doctor will wrap a band around the base of the haemorrhoid to constrict the affected area and stem the circulation of blood.
The result should be that the haemorrhoid, starved of blood and oxygen, will gradually shrink and fall off, usually within the space of a week.
Surgical procedures to remove haemorrhoids
Most cases of haemorrhoids can be treated through lifestyle changes, over-the-counter medications or non-surgical interventions. However, around 10% of people will eventually require surgery to remove them effectively.
Some of the most commonly used surgical interventions include:
Haemorrhoidectomy (haemorrhoid removal)
If medication or non-surgical procedures fail to treat your haemorrhoids, or you experience particularly large ones, a surgical procedure called a haemorrhoidectomy may be required to remove them.
This involves gently opening the anus to allow the haemorrhoids to be cut out. However, as the procedure is usually carried out under general anaesthetic, you’ll be asleep throughout and won’t feel any pain.
The area may be painful for a period afterwards though, but you’ll be given painkillers to manage this. After having it done, there’s also less than a 20% chance of the haemorrhoids returning, which is lower than with non-surgical treatments.
Stapling
Stapling, otherwise known as stapled haemorrhoidopexy, is often used as an alternative procedure to haemorrhoidectomy. It’s also often used to treat prolapsed haemorrhoids.
During the procedure, which is also carried out under general anaesthetic, part of the haemorrhoid tissue is removed before ‘stapling’ the remaining tissue in place inside the bottom.
This form of surgery has a shorter recovery time than traditional haemorrhoidectomy and also tends to be less painful.
Haemorrhoidal artery ligation
Haemorrhoidal artery ligation, otherwise known as HALO, is a form of surgery that's used to reduce blood flow to your haemorrhoids.
This operation involves using a proctoscope and specialist ultrasound probe to target the blood vessels supplying blood to your piles.
Once targeted, stitches are used to cut the blood supply, causing them to shrink over time.
As with all treatments and procedures, there are various advantages and disadvantages associated with each. So, if you think you might have haemorrhoids but don’t know which treatment option is right for you, consult your local pharmacist or doctor for their advice.
Remember, you can always ask to speak to your pharmacist in private to help you feel more comfortable talking about the condition.